Allen Lutz: Thanks for taking the questions. One for Craig. Can you bifurcate the relative growth rates you’re seeing in the acute and the non-acute GPO programs? And you mentioned there was market growth and then there was growth from further penetration. Can you break those two out? Thanks.
Craig McKasson: Yes. So I think as I talked about and Mike mentioned what we’re continuing to see in the acute part of the business is recovery at the kind of low-single-digit level year-over-year. And then non-acute is growing more at the mid to high-single-digit level and expectations that will continue into ‘24, low to mid-single-digit growth in acute overall gross activity and high single digit in the non-acute. In terms of market dynamics versus penetration, I don’t have a specific breakout, but I would tell you that the majority of our growth comes from continuing to drive same-store growth through contract penetration.
Allen Lutz: Great. And then last one for me. On the health system consolidation, can you talk about how that’s impacting the business this year versus maybe one, two or three years ago? Is it sort of a similar impact to the business? Or is it getting weaker or stronger?
Craig McKasson: Yes. What I would highlight is that in fiscal 2023, there was a very large merger of two of our significant with the Advocate Health merger. So I wouldn’t say that the overall activity is changing dramatically year-to-year, but I do think at points in time, the size and the magnitude of potential combinations can have a more significant impact one year over the other. So we’ll have to see as we look forward, which is why it’s — we don’t know who could be in conversations and what could happen. But the Advocate Health merger again, while both of them are premier members and continue to be committed to Premier engage with us in a lot of ways, it did have implications given the economics of those two accounts were different historically.
Allen Lutz: Thank you.
Operator: The next question is from A.J. Rice of Credit Suisse. Please go ahead.
A.J. Rice: Hi, everybody. Thanks for reviewing the history on the contract restructuring period. A lot of those contracts would seem to be coming up for renewal in the ’25 to ’27 time frame. Obviously, our modeling doesn’t necessarily go out that far. But if you’re in a strategic review process and people are trying to figure out what the long-term value of the entity is, it seems like to me, they’ve got to have a view on what’s going to happen in that ’25 to ’27 time period in terms of fee share changes or churn? I think in the investment community, it’s sort of perceived to be an open end to question, but maybe you have a better perspective. I wonder if there’s — I don’t expect you to quantify at this point. But do you feel like as you’re talking to people about different opportunities under the strategic review, you can give them some parameters, so they can assess what that looks like?
Mike Alkire: Yes, just — this is Mike. Just a couple of things. And I think, A.J., you could appreciate this. It’s challenging to predict what’s going to happen two to four years from now. I mean, especially as it relates to health care, especially as we’re coming out of a pandemic, it’s just one of those things that’s really tough for us to like put our arms around. Having said that, there’s a whole bunch of stuff that we continue to say and albeit Craig talked quite a bit about the pressures on the fee share from the macro environment and the different consolidation issues and some of those things that have been occurred. Our focus has always been the technology-enabled supply chain, right? And so what that means is, we want to continue to expand really the top line revenue, that gross admin fee number.
We think there’s incredible opportunity in the purchase service space, in the non-acute space. We do believe our Remitra offering is going to play a pretty significant role in terms of creating additional value for our health care systems. So — and just — in answer to your question, just in general, it is really hard for us given the puts and takes to put specific numbers out two, three, four, five years from now.
Craig McKasson: Yes, this is Craig. The only thing I think I would add, A.J., is that consistent with what we have told the marketplace. The market dynamics are challenging. There could be pressure on fee share in the future, and that’s something we’re continuing to evaluate. We have strategies to, as Mike described, to try and mitigate that as much as possible. But that’s something that has been a dynamic in the marketplace we’ve been consistently referencing.
A.J. Rice: Okay. Maybe my follow-up question. I’ll take the bait on the comment you made in the prepared remarks where you said you’re leveraging AI from purchasing to payments, looking at all the opportunities, maybe because we hear AI thrown around a lot. Are there some specific things that you’re using that for today to make the business more efficient or otherwise yield economics to you?
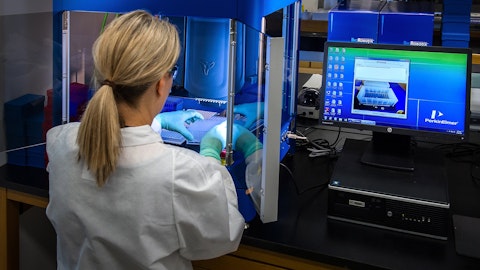
Mike Alkire: Yes. So a couple of different things. And Leigh is here as well, and Leigh can certainly jump in with any other additional commentary. But I think what’s really unique in that space is sort of the optical character recognition stuff that we’re doing on the invoicing and really bringing a great deal of meaning to that. So today, a lot of manual effort from a [Indiscernible] standpoint, we do think that we have some pretty unique algorithms sitting on our technologies that can actually automate a lot of those manual processes from a pricing accuracy standpoint, which is a significant burden for the health care system. So that’s one example. Leigh, I’m not sure if you have additional thoughts.
Leigh Anderson: I’ll just piggyback on what Mike said. There’s a concept computer vision, which is a field of artificial intelligence that enables computers and to sort of look at digital images. It’s sort of like the next generation of OCR, optical character recognition that Mike was talking about. We’ve been able to effectively use that to drive invoice recognition, and we’re trying to manage price for our members, and that’s really where we’re driving down on the artificial intelligence model for pick cure to pay.